In this topic, we continue our discussion of workers compensation on the Work Comp tab in Units At Risk.
The Classification Detail tab is used to manage classification detail and payroll information.
In the table that follows, we show you each of the buttons on the Classification Detail tab and its function.
|
Button |
Function |
|---|---|
|
|
Add a new classification record |
|
|
Delete a classification record |
|
|
Save changes to a classification record |
|
|
Save changes to a classification record and begin adding a new record |
|
|
Abandon changes to a classification record |
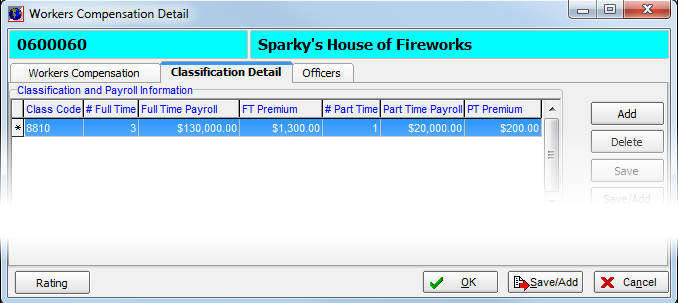
In the following steps, we show you how to add a new classification record. With practice, you can use the process that we show you to modify existing records.
- Click Add.
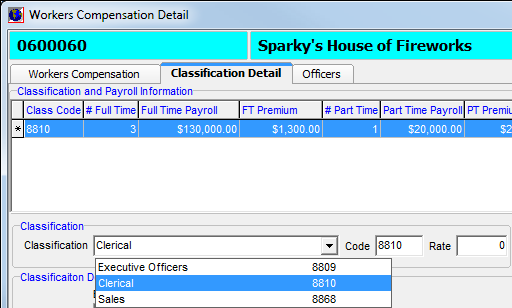
- In the Classification list, select a workers' compensation classification code. Selecting the code automatically populates the Code box.
|
Workers' compensation classification codes are a special type of rating code. They are managed in Data Maintenance Utility (DMU). The menu command to access the workers' compensation rating codes is not enabled by default. Please contact AIM Product Support for assistance enabling workers' compensation rating codes. |
- In the
Rate box, enter the percentage of payroll to automatically calculate premiums,
as shown below.
Alternatively, you can leave this set to zero and enter premium amounts manually.
- In the
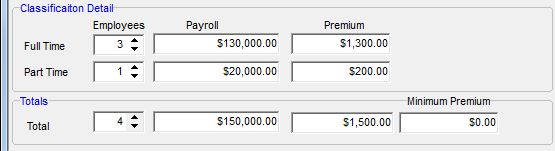
Classification Detail pane, enter information for both full-time and part-time
employees in the boxes provided.
Enter information for full-time employees in the Full Time row; enter information for part-time employees in the Part Time row.- Employees – Number of employees covered by the workers' compensation policy.
- Payroll – Total amount of payroll for covered employees.
- Premium – Premium amount to be charged for covered employees.
- In the Totals pane, verify the total amounts for the values that you entered in the Classification Detail pane.
- In the Minimum Premium box, enter a minimum premium amount, if applicable.